RESEARCH TRIANGLE PARK – Small innovations can make a big difference.
Just ask the people who work in WakeMed’ s neonatal intensive care unit. The hospital has installed NICVIEW cameras so parents of newborns can monitor their children’s progress from their personal smartphones. This has been a particularly valuable asset during the past year when COVID-19 protocols have limited personal hospital visits.
But there was a problem. The micro USB power adapters inserted into the backs of the cameras were unprotected and the cables would often break when the equipment was bumped or moved. So the cables had to be replaced regularly, resulting in additional cost, camera downtime, extra work for staff and potential inconvenience for parents. There are about 60 NICVIEW cameras in operation across the health system, so it wasn’t an isolated issue.

Jared Zimmel. — WakeMed photos
Enter Jared Zimmel, a biomedical tech specialist on WakeMed’ s clinical engineering team. The group is responsible for maintaining all the hospital’s equipment so that it meets health care standards and is operating properly. He drew the assignment of finding a solution to the micro USB issue. “It was an opportunity to branch off, be creative and do something different from the day-to-day stuff I’m used to doing,” he said.
Zimmel used an off-the-shelf computer design application and the department’s 3-D printer – purchased about a year ago to make replacement clips for headgear used in COVID-19 areas – to craft a plastic frame to protect the USB adaptor. It can be installed on the camera with existing hardware at a cost of only pennies per unit.
The printer can make three frames at a time over about a 13-hour period. Another plastic piece was developed with the same 3-D technology to hold the camera’s battery pack more securely in place, further reducing the strain on the micro USB cord. “It took us about 13 or 14 trials to dial in the frame design, but we’ve had no failures with the new equipment,” he noted.
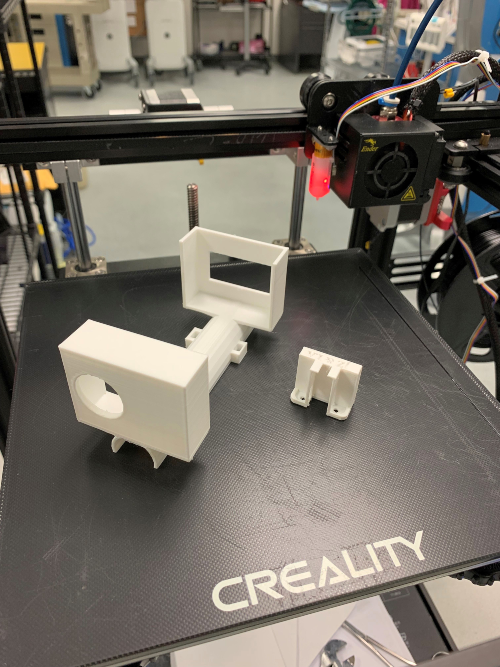
Devices created by Zimmel.
“These are just a couple of examples of the clinical innovations, both big and small, taking place within our hospital systems and health care organizations every day,” said Greta Brunet, who with colleague Corie Curtis started the North Carolina Biotechnology Center’s Clinician Innovation Initiative. Brunet, a former physician assistant, is senior director of investments with the Emerging Company Development team and Curtis is executive director of NCBiotech’s Greater Charlotte Office. “It’s this type of creative thinking we want to encourage and support to benefit patients and medical practitioners alike in North Carolina.”
NCBiotech and UNC FastTraCS are collaborating with WakeMed and 10 other healthcare systems across the state to do just that – turn good ideas into useful clinical innovations. A two-day virtual conference, Accelerating Health Care Innovation in North Carolina: Charting the Course, will connect participants with the people, insights and strategies they need to navigate the creative process, from ideas through execution. It will be held September 23 and 24 from 11:30 a.m. to 3:30 p.m.
The $25 cost of admission will include access to session recordings after the conference, as well as free admission to a separate Health Innovation Summit sponsored by Charlotte-based RevTech Labs on September 20-22. That event also is virtual.





























